Heart Sounds Training
What causes heart sounds?
Heart sounds are produced by two main mechanisms: 1) Sudden acceleration (or deceleration) of blood flow created by the opening and closing of cardiac valves or the tensioning of the heart's internal structures (e.g. chamber walls, or papillary muscles). 2) Turbulent blood flow created by unilateral protrusion into the blood stream, high flow rates, flows into abnormally large or small chambers or circumferential narrowing.
Abnormal heart sounds and murmurs can be found in infants or develop later in life.
Audio
Stethoscopes are used for auscultating heart sounds, often with chestpieces that include both a bell and a diaphragm.
Normal heart sounds resemble "Lub-Dub". These are the sounds of your heart valves closing normally. In some patients, the "Lub-Dub" sound is different, often with additional sounds being heard.
Heart Sounds and Murmurs
This fundamentals module for heart sounds and murmurs provides an overview of heart sound characteristics followed by lessons on twelve selected sounds. Each lesson includes text, heart sound recording and an anatomical animation of the heart producing the sound. These lessons are described below and also listed in the table of contents.
This website provides additional auscultation courses, reference guides, and quizzes. Certificates of achievement are also available.
Timing
Systolic murmurs occur after the first heart sound (S1) and before the second heart sound (S2). Diastolic murmurs occur between S2 and S1. In our lessons, timing phrases will be used to explain when murmurs occur within systole or diastole. For example, early systolic, midsystolic or late systolic.
Heart Sounds Location
Auscultation of heart sounds should be conducted carefully over at least five locations on the anterior chest wall. See the associated illustration for these locations. Many stethoscopes have chestpieces with both bell and diaphragm. Typically, start with the diaphragm but switch to the bell to hear lower-pitched sounds.
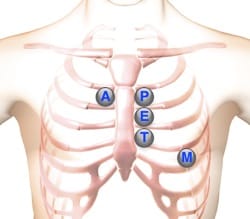
| Aortic Valve Area | Second right intercostal space (ICS), right sternal border | ||
| Pulmonic Valve Area | Second left intercostal space (ICS), left sternal border | ||
| Erb's Point | Third left ICS, left sternal border | ||
| Tricuspid Valve Area | Fourth left ICS, left sternal border | ||
| Mitral Valve Area | Fifth ICS, left mid-clavicular line |
Sound Duration
Heart murmur duration refers to the length of time of the sound. First and second heart sounds are short, while murmurs are typically longer. Murmurs lasting throughout systole are described as holosystolic or pansystolic.
Murmur Pitch
A heart sound's pitch (frequency) is an important characteristic. The observer should classify the sound or murmur's pitch as low, medium, or high. The stethoscope's bell can be helpful with low-pitched sounds, while the diaphragm should be used for medium or high-pitched sounds.
Loudness Patterns
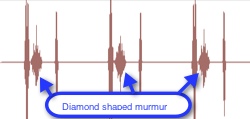
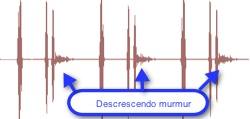
Heart murmurs are sometimes described by the pattern of the sound's loudness. Common classifications include crescendo (increasing intensity), decrescendo (decreasing intensity), crescendo-decrescendo (increasing then immediate decreasing intensity). Crescendo-decrescendo may be termed diamond-shaped. Finally, a heart murmur of constant intensity may be termed rectangular. Our lessons include waveforms images and videos that illustrate these loudness patterns.
Murmur Grades
| Grade | Description |
|---|---|
| 1 | Very faint |
| 2 | Soft, but readily detected |
| 3 | Moderately loud, no associated palpable thrill (a tremor or vibration felt on palpation) |
| 4 | Easily heard with associated palpable thrill |
| 5 | Very loud with associated thrill. Heard when stethoscope is placed lightly on chest |
| 6 | Very loud with associated thrill. May be heard with stethoscope entirely off the chest |
Tonal Quality
Additional aspects of the murmur's sounds can be used to characterize a murmur using terms such as musical, harsh, blowing, booming, sharp, or dull.
Patient Position and Respiration
Patient position and the respiratory cycle can alter heart sound splitting and murmur intensity. These factors are indicated within the heart sound lessons and our reference guide.
For each sound, we display the preferred patient position for auscultation.
Using Auscultation Lessons
Here we provide an example of a murmur. In this case, Aortic Stenosis.
Playback
Click the playback button on the torso to hear a short recording.
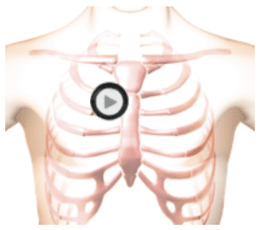
The patient was sitting during auscultation.
Phonocardiogram
A phonocardiogram is a plot of the sound's amplitude over time. Click the play button to view this phonocardiogram and hear the corresponding lung sound. This video will loop until paused.
Reference Guide
For subscribers, we provide a comprehensive heart sounds and murmurs reference guide. For each abnormality, one or more sound recordings are available along with text, phonocardiogram and cardiac animation.Start Fundamentals of Heart Sounds Course
Fundamental Heart Sounds
Introduction
Twelve heart sounds have been selected for of this introductory auscultation course. Each lesson, described below, includes a textual description, audio recording, and a video. Optionally, a quiz can be taken to measure comprehension and listening skills.
Normal Heart Sounds
The closure of the mitral and tricuspid valves creates the first heart sound. The mitral valve usually closes first, immediately followed by the tricuspid valve. Closure of the aortic and pulmonic valves creates the second heart sound.
This recording is a normal first and second heart sound with a rate of sixty beats per minute. The stethoscope's diaphragm is positioned at the apex (mitral valve area). Usually, the first heart sound is somewhat louder than the second heart sound when auscultating at the Apex. Sound intensity will vary with the chestpiece's position as well as with the patient's anatomy.
In addition to sound intensity, the first heart sound (S1) can be identified by its timing. At moderate heartbeat rates, the first heart sound follows the longer pause.
Normal Heart Sound - Lesson, Recording, Video
Splitting Second Heart Sound
When the aortic and pulmonic valves close, sounds are created. Normally a combined sound is heard, which is the second heart sound (S2). If these two components can be individually distinguished, the condition is called a physiological split.
Careful analysis of the splitting and intensity of the second heart sound can indicate the presence of many cardiac abnormalities.
While listening to the audio recording, observe that splitting varies between zero and eighty milliseconds depending on the respiratory cycle phase.
In physiologic splitting, the maximum separation between aortic and pulmonic components of the second heart sound occurs at peak inspiration.
In paradoxical splitting, the maximum separation occurs at peak expiration. Paradoxical splitting can occur with left bundle-branch block (LBBB) and aortic stenosis, both of which cause the aortic valve closure to be delayed until after the pulmonic valve closure, reversing the normal sequence of events.
Split Second Heart Sound - Lesson, Recording, Video
Fixed Splitting Second Heart Sound
When the separation of the two components of the second heart sound remains unchanged through inspiration, the split is called a fixed split.
The inability of the ventricles to change their volume with respiration causes the splitting. Fixed splitting of the second heart sound (along with murmurs) indicates the presence of heart disease or a heart defect.
Fixed Splitting Second Heart Sound - Lesson, Recording, Video
Third Heart Sound
A third heart sound (S3) occurs early in diastole, just after the second heart sound. S3 is a low-frequency sound best heard using the bell of the stethoscope pressed lightly on the skin of the chest. Position the chestpiece at the left lateral sternal border (LLSB) or xiphoid area.
Sudden deceleration of blood flow into the left ventricle from the left atrium causes the third heart sound. In the anatomy video, observe the thin-walled, dilated left ventricle with generalized decreased vigor of contraction.
In the presence of a third heart sound (S3), the first heart sound decreases in intensity while the second heart sound increases in intensity
In young people and athletes, it is a normal phenomenon. In older individuals, it indicates the presence of heart disease.
Third Heart Sound - Lesson, Recording, Video
Fourth Heart Sound
The fourth heart sound occurs in late diastole, just prior to the first heart sound. The fourth heart sound is a low-frequency sound best heard with a chestpiece bell pressed lightly onto the skin.
The fourth heart sound occurs during the diastolic filling phase, created by increased stiffness of the left ventricle, decreased ventricular compliance, or by increased volume. This may be a manifestation of heart disease. A fourth heart sound is never heard with atrial fibrillation because the contraction of the atria is ineffective in this condition. Review the anatomy video for an example.
The first heart sound is decreased in intensity and the second heart sound is increased in intensity.
Fourth Heart Sound - Lesson, Recording, Video
Innocent Murmur
Innocent murmurs are benign continuous sounds observed in pediatric patients with non-cardiac conditions such as pregnancy, hyperthyroidism, exercise, and anemia. When treated appropriately, the systolic murmur disappears.
Short duration and mid-range frequency characterize an innocent murmur. The stethoscope bell or diaphragm can be used.
In this recording, S1 and S2 are normal. Diastole is silent.
Innocent Murmur - Lesson, Recording, Video
Mid-Systolic Click
The mid-systolic click is usually created by the sudden prolapse of the mitral valve leaflet into the left atrium. The anatomy video illustrates this mitral valve posterior leaflet prolapse.
Listen to the recording of a mid-systolic click recorded at the apex. The first and second heart sounds are normal, and no murmur is present.
In some cases, a late systolic murmur follow the mid-systolic click.
Mid-Systolic Click - Lesson, Recording, Video
Mitral Valve Leaflet Prolapse
In this case, a mid-systolic click is immediately followed by a late systolic diamond-shaped murmur that runs to the end of systole. The intensity of the murmur increases and its starting point begins earlier in systole as left ventricular volume decreases (going from supine to standing).
On the anatomy video you can see that the murmur is caused by the prolapse of the posterior mitral valve leaflet. The murmur is represented by turbulent flow from the left ventricle into the left atrium.
Mitral Valve Leaflet Prolapse - Lesson, Recording, Video
Aortic Stenosis
This case presents a diamond-shaped systolic murmur associated with aortic stenosis. The first and second heart sounds are normal. The murmur starts in systole, shortly after the first heart sound and ends before the second heart sound.
The murmur is mid to high-pitched and is usually auscultated with the chestpiece diaphragm.
The anatomy video shows a markedly thickened left ventricle. The aortic valve leaflets are thickened and immobile. The murmur is caused by turbulent flow across the stenotic aortic valve.
Aortic Stenosis - Lesson, Recording, Video
Aortic Regurgitation
Aortic regurgitation produces a decrescendo murmur starting early in diastole. The first and second heart sounds are normal. The decrescendo murmur is high-pitched.
Aortic diastolic murmurs can be heard at the right sternal border, third and fourth intercostal spaces.
The anatomy video shows an enlarged left ventricle with normal contractility. Observe the regurgitant flow from the aorta into the left ventricle, which causes the murmur.
Aortic Regurgitation - Lesson, Recording, Video
Mitral Regurgitation
This case presents an example of a pansystolic murmur usually associated with mitral regurgitation.
The murmur is a mid-frequency, rectangular murmur taking up all of systole. S1 is normal. S2 is single. There is a third heart sound gallop in diastole. Both the left ventricle and the left atrium are enlarged. The murmur is caused by turbulent flow through the incompetent mitral valve leaflets into the left atrium.
In the anatomy video, observe the enlarged left ventricle and left atrium and turbulent flow from the left ventricle into the left atrium, creating the murmur.
Mitral Regurgitation - Lesson, Recording, Video
Mitral Stenosis
This case presents an example of moderate mitral stenosis. The first heart sound is increased in intensity, while the second heart sound is normal and unsplit. A diamond-shaped low-frequency murmur follows the opening snap. There is a second murmur in late diastole caused by the contraction of the left atrium. Use the bell of the stethoscope to hear this murmur.
In the animation, observe the turbulent blood flow from the left atrium into the left ventricle. Also, observe the moderately thickened mitral valve leaflets and the moderately enlarged left atrium.
This condition is most commonly due to rheumatic heart disease.
Mitral Stenosis - Lesson, Recording, Video
Course Quiz
After completing all lessons in a course, a quiz becomes available. If the user successfully completes a quiz, results are saved to the user's dashboard and a certificate can be printed.
Reference Guide
For subscribers, we provide a comprehensive heart sounds and murmurs reference guide. For each abnormality, one or more sound recordings are available along with text, phonocardiogram and cardiac animation.Authors and Reviewers
-
Heart sounds by Dr. Jonathan Keroes, MD and David Lieberman, Developer, Virtual Cardiac Patient.
- Lung sounds provided by Diane Wrigley, PA
-
Heart sounds mentorship by W. Proctor Harvey, MD
- Reviewed by Dr. Barbara Erickson, PhD, RN, CCRN.
-
Last Update: 11/10/2022
Sources
-
Heart Sounds and Murmurs Across the Lifespan (with CD)
by Dr Barbara Ann Erickson
Publisher: Mosby
ISBN-10: 0323020453; ISBN-13: 978-0323020459 -
Heart Sounds and Murmurs: A Practical Guide with Audio CD-ROM 3rd Edition
Elsevier-Health Sciences Division
Barbara A. Erickson, PhD, RN, CCRN -
Heart and Lung Sounds Reference Guide
PracticalClinicalSkills.com -
Heart Sounds Made Easy with CD-ROM: (with CD-ROM) 2nd Edition
Anthony P. Salmon
ISBN-13: 978-0443069079 - NCBI Review of Heart Sounds and Murmurs: A Practical Guide
-
The Virtual Cardiac Patient: A Multimedia Guide to Heart Sounds And Murmurs
Jonathan Keroes, David Lieberman
Publisher: Lippincott Williams & Wilkin)
ISBN-10: 0781784425; ISBN-13: 978-0781784429 -
Ventricular Function Curves in the Exercising Dog
JONATHAN KEROES , ROGER R. ECKER , and ELLIOT RAPAPORT
Circulation Research, Vol. 25, No. 5 -
Electrocardiographic changes associated with ritodrine-induced maternal tachycardia and hypokalemia
American Journal of Obstetrics Gynecology, VOLUME 154, ISSUE 4, P921-923, APRIL 01, 1986
Susan K Hendricks, MD, Jonathan Keroes, MD, Michael Katz, MD -
The_Virtual_Cardiac_Patient_A_Multimedia_Guide_to_Heart_Sounds_and_Murmurs
A Multimedia Guide to Heart Sounds and Murmurs
January 2007 JAMA The Journal of the American Medical Association 297(2):217-218
DOI:10.1001/jama.297.2.217. M. Saleem Seyal, MD, Reviewer -
Clinical Heart Disease
W Proctor Harvey, MD
Laennec Publishing; 1st edition (January 1, 2009)